|
I was originally diagnosed with PCOS in 1987. In 1997 I was diagnosed with DDD @ the L4/L5
& L5/S1. In 2004 I was found to have DDD @ the C4/C5 & C5/C6, along with Fibromyalgia. December of 2004
I was diagnosed with Uterine Cancer. I had a hysterectomy in February 2005. After a biopsy was done, it was found
that I had Endometrial Cancer and Endometriosis.
I have been living with severe pain nearly every single day of my life since 1986. This page
is my story of living with daily Pain.
What PCOS Has Done To Me
by Bren Hadjian
May, 2004
I remember the first time I had a period. I thought I was dying. I was 12 or 13 years old and woke up to a nasty mess.
Mother explained to me that it was a normal process a woman goes through every month. I was going to live.
By the time I turned 14 they stopped all together. All through high school I was period-free. I mentioned to my step-mother
that my monthlies stopped. She said I needed to see a doctor and that a doctor would probably put me on birth control to regulate
my monthlies. She never took me to a doctor.
At 15 I brought it up with my father, telling him what my stepmother had said the summer before and that I needed to see
a doctor. Still nothing. I left that home as soon as I turned 18.
I was into weightlifting, working out regularly at Hilltop (a gym). I was proud of my 5'5", 135 pound self. I thought I
looked great. No one loved me like I did. I was strong, healthy and happy. I had nice legs, too.
Early 1987, I started having low abdominal pains while at the gym. Sharp pains to the left or right. Then I started gaining
weight. I freaked out. I did not want to get fat. I worked out more. I still gained weight. The pains were horrible. I quit
eating. It never occurred to me that it would be related to the fact I never had periods any more. The pains got pretty severe
and a friend of mine talked me into seeking medical attention, fast.
I went to a clinic in Kansas City. During the first 3 visits I saw 5 different doctors and got 4 different diagnosis's.
I was prescribed birth control pills and 1600 MG of Ibuprophen 3 times a day for pain. The Ibuprophen decimated my stomach.
I was given Percocets for the pain. I kept gaining weight. Depression was becoming a problem. A laporoscopy was done and it
was confirmed. I had Polycystic Ovarian Syndrome (PCOS). In 1987 & 1988 there was very little information about PCOS.
I was told I would never get pregnant. My hormones are out of whack. I was told I needed to lose weight. I was losing the
hair on top of my head but gaining it every where else. (Ninety percent of what I know now I learned from books, magazines
and the internet.) I felt like a freak of nature. A beast.
I tried to lose the weight. The weight was extremely resistant. I gave up. I have tried every diet known to man. I tried
diligently to get pregnant. I was an emotional wreck. After several years of taking BC pills, my periods stopped again. I
went four years without one. One day out of the blue, I bled like a stuck hog. Forget the pads and tampons. I was using towels.
It lasted only a couple of hours then quit. I didn't have another for several months. (As of this writing, it has been over
three years since the last period.)
On my next annual exam, the doctor told me I was pregnant. You have got to be kidding me? He figured me to be two months
along. I was elated. I went shopping. My husband at that time was not as thrilled as I was. This was a major hurdle for me.
An ultrasound was done. I was happy. I was going to have that baby I was told I would never have. Shortly after my third month
the doctor told me my body absorbed the baby. I called him a liar. I said it wasn't possible. How could my baby just disappear?
I told myself I was never pregnant. I convinced myself I was never pregnant. I believed it for several years. I tried Clomid
(a fertility drug). It did not work. I have begged many doctors, "If my stuff is not going to work, then get it out of me.
I want a hysterectomy." They kept telling me not until I have a baby, cancer or am older. This always enrages me. I
cant have babies. I don't want cancer. I'd truly like to AVOID cancer! What does age matter? My stuff has not worked since
I was 14 years old. Did PCOS take my age into consideration? No!
For years I stayed away from everyone who had or was having babies. I was insanely jealous of them. I am not as jealous
now. Years has made me appreciate what I do have. My heart aches for the one I lost. I will be 37 here in a few days. Too
old, I feel, to even try to have any baby. I have no sex drive left. I am no longer married. I dont want to date. PCOS has
left me feeling like a short, fat, hairy he-she. A true freak of nature.
* If not treated properly, PCOS can lead to other, more serious conditions. If you suspect that you may have
PCOS, consult with your OB/GYN.
December, 2004 - Uterine Cancer was discovered.
January, 2005 - After more Doctor Visits, it was learned that I have been having "monthlies".
Problem is I have been "discharging" into the pelvic region, instead of through vaginal discharge. I have to have surgery,
a total hysterectomy.
February, 2005 - Surgery. A biopsy was performed after the surgery and Endometrial Cancer
was found. It was discovered that I, also, had a "severe case of Endometriosis".
Degenerative Disc Disease.
by Bren Hadjian
May, 2004
As I stated earlier (Fibromyalgia article), I was diagnosed with Degenerative
Disc Disease (DDD) in 1997, after a work-related accident, at the L4/L5 & L5/S1 levels with disc bulging at L5/S1.
It was determined the accident did not "cause" the DDD, but had "exacerbated" it. Workman's Comp released me in 1999.
For years I have suffered severe, often dibilitating, pain, most
of which I "assumed" was because of my DDD in the Lumbar region. Several doctors said it wasn't, i.e. the Fibromyalgia
diagnosis last week. Two MRI's were done last week, Cervical and Lumbar. I got the reports today (5/14-2004).
I now have, in addition to the above, DDD at the C4/C5 & C5/S1 with disc bulging at both, bulging at L4/L5 AND nerve
root damage, right and left side of L4/L5/S1.
I asked the doctor what did this all mean, am I going to be paralyzed?
He responded that it would not be the bulging lower discs that paralyzes me. He thinks I need more epideral shots, even
though they did not work in 1997-8.
I think I need another doctor.
My Experience on July 7th & 14th, 2004.
I am in the process of trying to get disability. I have already been deemed disabled by the
state. (SSA takes longer.)
A little case history first.
In
1997-99 I had an accident that resulted in me being diagnosed with Degenerative Disc Disease (DDD) @ L4/L5, L5/S1 with Disc
Bulging @ L5/S1. From 2001 until now I have been having serious pain and swelling which has driven me to the emergency rooms
and numerous doctor visits. One ER doctor told me I needed to get my back reevaluated (new MRI) which is why I was referred
to the Headache & Pain Ctr in Leawood, KS. After the new MRI, I was diagnosed with additional DDD @ C4/C5, C5/C6 with
Disc Bulging @ both and Nerve Root damage Left and Nerve Root damage Left and Right @ L5/S1. I, also, have PCOS, Diabetes
(Insulin Resistance), Fibromyalgia and suffer from blinding migraines (for which the cause has not yet been found. I suspect
the bulging discs. The kind of Migraines that make you wished you could die.) I have a 2 1/2" binder full of medical records
showing all the treatments and physical therapy I have had and Doctors recommendations indicating that no physical therapy,
no Epidural, no trigger point injections, would be beneficial at this point in time. I was at my maximum level of recovery
(Dated 1999). (This was to end the Worker's Comp thing.) All I wanted was to go back to work. That's all I still want is to
go back to work. Per conversation with a Social Security Staffer who noted that I had worked steadily from 1983 until 2000,
three years after I was originally injured.
However, since 1999, it is safe to say that the amount of DDD has doubled.
The amount of pain I have to live with on a daily basis has reached unbearable.
Now
for the matter at hand ...
... on the 7th of July, 2004, I went in to see Dr B (this is like my 3rd
or 4th visit) @ the Headache & Pain Ctr in Leawood, KS, per a referral from my GP, and told him what Dr D (GP) said on
the 2nd of July, and that was that he never meant for me to see a neurologist. Dr B said then "if it was a pain specialist
they meant for you to see then we can arrange that". After an EMG was performed, I was seen by a pain specialist who I swear
is INCOMPETENT!
This INCOMPETENT (Dr MA G) is telling me I have limited choices. Epidural or trigger point injections.
I said No. What about Spinal Fusion. He said I "didn't have enough nerve damage to warrant surgery". He was explaining
to me that I had DDD because I smoked, was overweight and getting old. This really angered me because #1: I was originally
diagnosed with it in 1997 at the age of 30 (and then it was said to be a "pre-exsisting condition"). #2: I wasn't always overweight.
As a matter of fact I used to be really, really cute. Back when I could move and was really flexible. I was thin and cute
and vain, but cute. #3: I am now only 37 years old. At 30 I was told by an Orthopedic Surgeon that I had the back of a man
in his 70's and that it was a "pre-exsisting condition exacerbated by the accident at work". (This is DOCUMENTED, which I
carry in my binder to my doctor visits.)
After several minutes of arguing with him. I caved. I agreed to the Epidural
to prove to him they don't work, because I've had it before and I had brought him proof I've had it before but he said that
was in the lumbar not the cervical, it could be different. Two nurses came in. One swabbed the back of my neck with an alcohol
swab. The other then called the Dr back in. He gets on my back (which is riddled with pain), jabbs his thumb above the injection
site hard and jabbs this freaking needle into my neck. This one not only did not work, but gave me a horrible headache and
made me very sick. Pain surged through my upper back, shoulders and arms. After 30 minutes I was sent home. I had to drive
from Kansas to Missouri through road construction and rush hour traffic on I-435 to I-35. By the time I got home I had a slight
bruise and swelling at the injection site.
Once I got home I called and asked if I could take anything for the horrible
headache and was told someone would call me back. No one did. I took Percocets and the rest of my meds. The next afternoon
someone finally called back and I said don't bother I took matters into my own hands then hung up on them before I said something
I would later regret. The following week I went in and he was going to give me another. I told him he was not going to touch
me with another. I said there was no way you are coming near me with another. My neck was still swollen from the last one.
He looked at me stupid-like then turned to the computer and said "then we need to come up with a plan c d e &
f." He said "looking at your EMG you have no nerve damage. That is good". He tripled the dosage of seizure meds and
hands me what was supposed to be my EMG report and new script then leaves. What I had in my hand was another woman's MRI of
her brain. Clearly labeled and marked. Two copies. I started raging.
I'm telling my Psychiatrist about this last week
and I showed him what that DR gave me and he's looking at it and his eyes got huge. He said, "do you know how many laws this
Dr has broken?" < HIPPA >
I called the clinic up and asked the manager if I could have that woman's address and phone number
and she said, "the doctors know what they give their patients and it is unlikely he would have given you ..." then I started
reading it to her and she shut up for a long little bit. Then she asked me what are you going to do with it. I said ... All
I've been trying to do is talk to Dr B since Friday. That's it. Now I am going to go online and I am going to find this woman
and I am going to tell her what that DR gave me.
My problems are these:
This DR was looking
at an MRI Brain scan of another woman (clearly labeled) and telling me that my EMG shows I do not have nerve damage there
fore there is nothing seriously wrong with my back.
This is the same DR that got onto my back and jabbed an Epidural
into my cervical spine without any painkillers or numbing agents, as per the Step-by-Step Directions I found. I have had a horrible dread of needles, supposedly since infantcy (Mother's story). I make sure all
doctors know this. To prove this point, the one time I had to have cavities filled the dentist did so without any shots of
Novocain.
My Psychiatrist was telling me I should go back to that clinic and show this DR what he has done. I told
him I will not go back because if I do I just might hit that DR.
Dr B, who I really liked and thought was a good Dr,
has never returned any calls. (I really liked him because it seems he has been able to cut drastically the number of migraines
I have.)
Should the other woman be made aware, as I have not been able to find her?
I have yet to see my EMG
results.
Here it is July 28th and my neck is still hurting at the injection site. The pain is actually worse than when
I originally went in.
I want to know what can be done about this! I think this is serious.
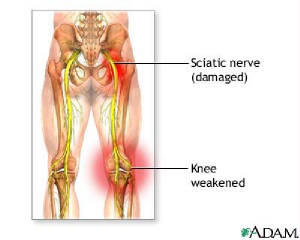
| This picture from Adam clearly depicts ... |
|
| the "Garden Hose" I complain about in my butt and legs. |
My Life with Fibromyalgia
by Bren Hadjian
May, 2004
Where do I start? My back? Legs? Arms? Maybe my neck? The pain is all over. From head to toe. I have a myriad of symptoms
that I have suffered with for years. I have complained about the pain so much nearly everyone I ever knew has walked away
from me. Family and friends alike. Now I have tacked on loneliness to the many symptoms of my Fibromyalgia. Most can not relate
to the kind of pain I endure day in and day out. No one wants to hear about it.
The pain started in September of 1997. I had a little slip and fall accident at work. I did not think it was anything
serious. Until the next day. I called my building supervisor and asked him for the following day off so I could give my back
a break. He ordered me to the Workers Comp Group. To this day, I feel my nightmare began there. The nightmare called Fibromyalgia.
I went as ordered. I did not want to. I truly felt I would be fine with some time off and rest. The first round of
Workers Comp Doctors gave me a lifting restriction, which lead to three weeks off work, prescriptions for pain and muscle
relaxers and diagnosed me with a back sprain. Cool. That is all I thought it was to begin with.
Time passes and the pain is getting worse. I can barely get around. I tell these Workers Comp doctors this. Days later
I get a phone call from a contracted Nurse/Case Manager (French). I liked him until I met him. He set up an appointment for
me with some very popular Orthopedic Surgeon. I'll call him Dr. P. Every two to three weeks this doctor was giving me different
medications. Antidepressants. Anti-inflammatories. Nothing for the pain. Finally, after several months of this torture, an
x-ray was ordered. Dr. P. came back and said I had Degenerative Disc Disease. He put in his little report that it was not
caused by the injury from work. It was pre-exsisting.
Meanwhile, new medications every visit. I kept getting sicker and sicker. I started having black outs. By August of 1998,
I was so depressed and the pain was so intense I could not take it any more. I tried to end it. I swallowed every
pill I had in the house. OTCs and Prescription. I swallowed them all. Then I started vomiting. The vomiting seemed to last
forever. My gut hurt. My head throbbed. My jaw ached. Weak and crying, I sat on the floor. This is how my boyfriend, at that
time, found me.
I had to go on a medical leave from my job. I could no longer do the functions of that position. I found a part time job
I could do. It gave me the freedom to move around or sit. I discovered Xenadrine RFA. It was a dietary supplement, with Ephedra.
I started taking it and after a couple weeks I felt as though it really helped with my pain. I could move around. I was happier.
I was even losing weight. Later, I was told that Ephedra was not helping. I still don't believe it.
My Workers Comp Case was forging on. I had to retain an attorney. I felt as though my Nurse/Case Manager and Dr. P. were
screwing me around. The lawyer arranged for new doctor appointments and, eventually, a new case Nurse/Case Manager. .
Five doctors later and an agreement on diagnosis. Dr. F. told me that I had the back of a man in his 70s. Bear in mind,
I was a 31-year-old, Caucasian Female. Back surgery was not recommended at that time. Dr. F. explained to me that I had Degenerative
Disc Disease at the L4/L5 & L5/S1with Disc Bulging at the L5/S1. He went on to say that no amount of Physical therapy,
Steroidal Injections and pain killers was going to alleviate the pain. He said I had reached maximum improvement. "It is as
good as it is going to get."
I changed jobs again. I eventually quit the job I was injured at. I could no longer perform the physical aspects of the
job. Depression got worse. I started having panic attacks. Finally, I had to make changes. I moved to Oregon. I tried to procure
employment there. It was fruitless. I worked a few part time, temporary jobs, finally landing a temporary job at the post
office as a Data Entry Clerk. That position ended after 6 months and I was retained as a Mail Handler. I swore I could do
that job. By the end of the first night as Mail Handler my legs and feet hurt worse than ever. By the end of the first week
I wanted to die. I made it 4 weeks before I was forced to quit. The swelling of my hands, legs and feet would not go away.
I had to have help getting out of my van once I got back to the house. Embarrassingly enough, I even had to have
help with toiletries. Here I was broke and depressed, in Oregon. I tried to make the best of it. I wound up coming back to
Missouri.
The pain got worse in 2002. This was the worst pain I had ever experienced in my life. Or so I thought. I was experiencing
short term memory problems. I was not functioning with a full deck of cards. I couldnt sleep. The shooting or stabbing pains
would wake me every hour or two. I started having chest pains. I really believed I was having a heart attack and dying. I
was hospitalized for 2 days with the chest pains, while medical personnel performed routine tests. My white blood cell count
was high. Other than that they could find no reason for the chest pains. They decided it had to be acid reflux. I said, "No
way!" I walked out of the hospital, against doctor's orders. I felt I was not being taken seriously. Recently,
I learned that NonCardiac Chest Pain is common in Fibromyalgia.
My DFS Case Manager set me up for doctor appointments for a disability rating. First I was sent to an Orthopedic Doctor,
who said my complaints did not coincide with diagnosis. He suggested I see a Psychiatrist. Then I was sent to a Psychiatrist
(which I thought was lame, as I was already seeing one.) The Psychiatrist said my problem was physical. So I did not qualify
for disability.
During the Summer of 2003, temperatures hit above 100 degrees. The higher the temperatures, the more I swelled up. I went
to the hospital three times because of the swelling alone. First my feet were swollen so bad it hurt to walk on them. Another
time my legs and feet swelled. The third time I went I was swollen from the waist down. I was so swollen could not wear pants
or shorts. No causes were ever found. The swelling was attributed to my weight.
Still unemployed. No money. Homeless. Depression at an all time high. My kids are keeping me going. They
do not understand the severity of what is going on with me. I started keeping a pain journal. I recommend anyone suffering
with chronic pain do this. My first pain journal was a simple calendar that I carried in my purse. I noted the days the pain
was the worst. Believe me when I say, this will come in handy. I made notations of where the pain was and sometimes I tried
to describe it. Describing pain, for me, is hard. I dont know much how to describe pain other than, "It Hurts!" I am
learning though. When dealing with doctors, it is imperative that you know the right adjectives to use when describing pain.
The headaches turned into horrible migraines. Some of the migraines would last five to seven days. No OTCs worked. I finally
went to the clinic. I was given Fioricet, Relafen and something else (I cant remember what it was). None of it worked. I called
the clinic back and told them my head hurt so bad that I was having black outs again. I was instructed to go in. I said I
couldnt drive. I was, then, instructed to go in when I could.
I typed up a letter to the doctor explaining my history with the pain. It took a few days, due to memory problems, but
I got it done. It was lengthy. I explained every detail I could remember. Every medical test performed and results. My sister-in-law
had gotten some information on Chronic Fatigue Syndrome or CFS. I took my letter and the information to Dr. D. I explained
to Dr. D. that I was in serious pain. I can't go on living like this. He was at a loss as to what to do. He arranged for me
to start water physical therapy and prescribed me 60 MG Inderal LA (a blood pressure medication) to help with the headaches
and migraines. I, also, got Stadol NS for the migraines. Stadol NS works great for me. Because Stadol is so hard to
get due to how addictive it supposedly is, I use it only if the migraines are at the utmost worse. I am proud to say, after
two months on the Inderal, I have had one migraine and a few small headaches that didnt require any medications. Now if only
I could find something that could help with the rest of the pain that runs rampant throughout my entire body.
A couple of days after that doctor visit, I was struck with a new pain. One I had never experienced before. It felt as
if when I sat or laid down I had a garden hose tucked away in my left butt cheek and thigh. It hurt. Oh my goodness, did it
ever hurt. After a couple days and nights of that and trying to call my doctor, with no success, I went to the Emergency Room.
It was determined there that my sciatic nerve was being pinched and inflamed. I was told it was time to get my back re-evaluated
for possible back surgery. I tried for three weeks to get a hold of my doctor, leaving several messages and getting no return
calls. Even the pharmacy tried calling about refills and they, too, received no return calls. It was dismal. I had this garden
hose thing going on for the entire three weeks of physical therapy. Along with a new pain.
During my second day of PT I had an asthma attack in the pool. The asthma attack led to a violent coughing spell that created,
yet, another pain in my chest, right behind my right breast. It felt like muscle was being ripped inside me. It hurt to breath.
It hurt to move. I could not lay down. I cried a lot. It hurt to raise my right arm just a few inches.
One woman told me to ask my doctor about Fibromyalgia. She said I acted a lot like her other Fibromyalgia patients. When
I got home I got online and started my own research. I couldn't believe what I was reading. Never in my life did I expect
to see something that accurately depicted what I have gone through over the last seven years. It brought tears to my eyes.
I read about other peoples accounts of Fibromyalgia. The pain they, too, have suffered. One description I read was something
I had said many times over the last seven years. I wake up in the mornings feeling like I have been run over by a Mack truck
- twice. I burned up a lot of paper and ink printing Fibromyalgia information off.
I collected medical records from past doctors visits (which took three months to collect). At my next doctor visit with
Dr. D. I produced all the information I had collected since the last visit. I gave him time to read my newest letter. When
he was done I said, I have brought proof that I have been suffering severe, debilitating pain for the last seven years. Something
has got to be done about it. I can't take it any more. He said he never doubted I was in pain. I told him of my Fibromyalgia
research. I said to him, "This is the only thing I have found that accurately depicts what I have
been going through these last seven years.' He said to me that if I had to put a name on what was wrong with me it would
probably be that. But he was not comfortable with it because Fibromyalgia can not be detected by blood or urine tests or x-rays.
Fibromyalgia is diagnosed by ruling every other possible cause out. According to the medical records I brought with me to
that visit, everything else had been ruled out. Dr. D. referred me to the Headache and Pain Center to have my back re-evaluated.
The appointment was made for a couple days away.
I made it to the Headache and Pain Center. While there, I was attended to by a Dr. B. Dr. B. went over my medical history.
I showed him my past reports from other doctors. He had me stand up. He grabbed my neck, "Ouch!" He grabbed my elbows,
knees, low back, "Ouch! Ouch! Ouch!" He said you have tenderness at the tender points. I showed him my pain journal
with my pain charts. He said you have Fibromyalgia and that I should have been referred to a rheumatologist. Dr. B. arranged
for the upper and lower MRI's to re-evaluate my back.
Now I know why I hurt. I know there is no cure. What matters the most is it is no longer just all in my head. It is something
that I will have to learn to live with. I will have to learn to function with. I suffered for 7 years before anyone could
or would tell me what was wrong with me. The pain of Fibromyalgia affects everyone differently. Some people can still go on
with their normal lives. Others are left writhing in the worst of pain. Suffering and often praying to die.
I don't want to die. I want to live. Preferrably pain-free.
"Doctor, I need the BEST pain killer!"
|

